What is Frozen Shoulder?
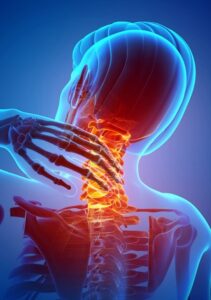
Everyone has heard of the term “Frozen Shoulder”, but what in actual fact is it? Put simply, it is an inflammatory condition which causes pain and stiffness of the main shoulder joint (the gleno-humeral joint).
The term “frozen shoulder” is often used incorrectly as a generic term describing any condition that causes stiffness in the joint and is something of a layman’s term, but it is a real condition, whose name is Adhesive Capsulitis.
Adhesive capsulitis may occur following minor trauma, such as a mild strain, and causes inflammation of the flexible lining of the joint, known as the joint capsule. Inflammation of this structure causes a thickening of the tissue, making it like a tight elastic band, which then limits movement and results in pain.
How is Frozen Shoulder Diagnosed?
Most commonly, patients complain of pain, which they have often had for several weeks. Subsequently there follows a period of stiffness which limits the range that people can move their arm comfortably. This can be quite disabling.
The first ranges of movement affected are when you move your arm away from your body, either sideways or to the front. Also rotating your arm, e.g. to put a coat or shirt on, or trying to fasten a bra will be painful.
Typically a pattern develops which the condition follows, consisting of three phases:
Phase 1- Freezing: this is painful and can last 2-9 months.
Phase 2- Frozen: less painful but increasingly stiff. This phase typically lasts 4-12 months.
Phase 2- Thawing: gradually less pain and stiffness- a period over which symptoms settle.
What are the symptoms of frozen shoulder?
These will include: Pain, Stiffness, Difficulty sleeping, Inability to lay on the affected side.
How common is Adhesive Capsulitis?
Frozen shoulder will affect 5% of the population at some point in their life. Most commonly it tends to be particularly prevalent in middle age (peaking between 40-60 years of age) and affects women slightly more than men. Scientists therefore believe that there may be a hormonal influence affecting the condition which has an effect on the connective tissues.
What causes Frozen Shoulder?
Studies tell us that minor trauma may be the trigger to start the process of developing frozen shoulder. Repetitive actions in sport, such as throwing, racquet sports and swimming may increase the risk. In actual fact, it is still unknown as to why people develop the condition, but other risk factors that have an influence include:
- Diabetes
- Heart Disease
- Connective tissue disorders, such as Dupytren’s contracture (thickening of the skin of the hand).
What are other common shoulder injuries?
A skilled manual therapist or GP should be able to diagnose a frozen shoulder without the need to further tests. Their history and physical examination should be enough to go on. Our team of osteopaths in our Surrey (Woking and Hinchley Wood) clinics, or our main Wimbledon practice, will help you reach an accurate diagnosis.
Commonly the condition is misdiagnosed as being:
- Tendonitis
- Muscular strain or tear
- Damage to the lining lip of the shoulder joint (glenoid labrum)
- Calcium deposits in local soft tissues
What is the best treatment for Frozen Shoulder?
- Do nothing! The condition is generally self-limiting, meaning that it will pass naturally in most cases after a period of several months or years. However, most people find it unacceptable to have this level of pain and stiffness.
- Manage the pain and inflammation with over the counter medication
- This may not be enough, so some opt for prescription medication
- The treatment of choice in my opinion is to have conservative manipulative manual therapy, such as osteopathy or physiotherapy. The aim is to reduce the swelling, maximise the joint range of motion and to treat the surrounding (compensatory) regions.
- Steroid injections in the past have been a popular route for some clinicians, but increasingly less common these days.
- Hydrodilatation- stretching of the joint capsule by injecting a large volume of fluid into it.
- Surgery- if you are brave, you can try a manipulation under anaesthetic, or increasingly popular with orthopaedic shoulder specialists these days, a process called Capsular Release, which involves using a radio-frequency probe to release the tight joint capsule.